Introduction
Managing medical inventory is a critical component of running any healthcare facility, from small clinics to large hospitals. Medication, medical supplies, and equipment must be available when needed—yet not so overstocked that they expire or waste precious budget. Poor inventory management in healthcare can lead to dire consequences. For example, hospitals collectively discard an estimated $765 billion worth of usable medical supplies each year due to inefficiencies, and roughly 7–10% of inventory items end up expiring on the shelf unused. Such waste not only inflates operational costs but also risks patient safety if expired products are accidentally used. Even smaller clinics are not immune to these challenges; lacking the right inventory management system can result in stockouts of critical items or costly overstock.
Effective healthcare inventory management ensures the right supplies are on hand at the right time while minimizing waste. This directly impacts patient care and the bottom line. Studies have shown that nearly 40% of healthcare staff have had to cancel or delay procedures due to out-of-stock supplies. No medical practice wants to tell a patient their treatment is postponed because a crucial item wasn’t in stock. Additionally, inventory often represents a significant portion of expenses—industry data indicates at least 20% of a typical hospital’s budget goes toward pharmaceuticals and medical supplies. For clinics and healthcare businesses operating with tighter margins, optimizing inventory is essential to controlling costs.
In the following sections, we outline common challenges of medical inventory management and provide essential tips to overcome them. By implementing a robust clinic inventory management system and following best practices, healthcare businesses can streamline operations, reduce wastage, enhance compliance, and ultimately focus more on patient care than on counting supplies. The tips below will help clinics and other healthcare organizations maintain an efficient inventory management process that supports excellent care delivery and sound financial performance.
Why Effective Inventory Management is Critical in Healthcare
Inventory management in healthcare is about more than tracking supplies – it’s about ensuring patient safety and operational continuity. Healthcare providers must manage a wide range of items, including medications, syringes, personal protective equipment, diagnostic tools, and more. If any of these run out or are unusable, the quality of care suffers. For instance, using an expired or recalled product can put patients at risk, potentially resulting in ineffective treatment or safety incidents. Proper inventory control helps prevent such scenarios by removing expired items promptly and monitoring recall alerts to pull unsafe products from use.
Moreover, efficient inventory management for clinics and hospitals supports financial health. Overstocking ties up capital and storage space, while understocking can halt services or force expensive last-minute purchasing. Striking the right balance means the facility has neither too much nor too little of each item. It also aids compliance with various regulations. Healthcare is a highly regulated sector; maintaining accurate inventory records and traceability is necessary for audits and accreditation standards (for example, tracking lot numbers of medications for safety and recall management). An organized inventory system helps clinics remain compliant with health regulations and quality guidelines, avoiding penalties for missing documentation or improperly managed medical supplies.
Finally, inventory efficiency improves overall staff productivity and patient satisfaction. When supplies are well-managed, clinicians and nurses spend less time hunting down items or handling paperwork and more time attending to patients. Shortages that delay procedures or force staff to improvise with alternatives can frustrate both providers and patients. In summary, an effective medical inventory management strategy ensures that patient care is never compromised by supply issues and that the healthcare business operates smoothly and cost-effectively.
Common Challenges in Medical Inventory Management
Implementing good inventory practices in a clinic or any healthcare setting comes with challenges that need to be addressed:
- Overstock vs. Stockouts: Without proper oversight, clinics may overstock some items (leading to waste through expiries) while understocking others (leading to dangerous shortages). Managing the balance is difficult without a systematic approach. Excess inventory can expire or become obsolete, while missing supplies can disrupt treatment schedules.
- Manual Tracking Errors: Many smaller healthcare facilities still rely on manual methods like spreadsheets or paper logs to track inventory. Manual processes are error-prone – numbers can be entered incorrectly or not updated in time. Such errors cause discrepancies that lead to ordering mistakes or items not being where they’re supposed to be. In multi-department clinics or those with multiple sites, manual tracking often fails to provide a real-time, consolidated view of inventory levels.
- Limited Staff and Time: Clinics often have clinicians or administrative staff doubling up as inventory managers. Staff shortages or busy schedules can result in inventory checks being neglected. Without dedicated tools and processes, keeping inventory organized may fall through the cracks during hectic periods, resulting in disorganization or forgotten tasks (like reordering or removing expired stock).
- Lack of Visibility and Data: Inventory data spread across different systems or recorded inconsistently makes it hard to get a clear picture of usage patterns. This lack of visibility means the clinic cannot easily forecast demand or identify inefficiencies. It also hampers communication between departments – for example, if one department doesn’t know another has spare stock of an item, they might reorder unnecessarily, leading to duplications.
- Supply Chain Disruptions: External factors like supplier delays, medication shortages, or sudden spikes in demand (as seen during the COVID-19 pandemic for items like PPE) can wreak havoc on a clinic’s inventory. Clinics need systems and plans to quickly adjust to such disruptions, such as finding alternate suppliers or redistributing stock internally. Without preparation, a clinic can be caught off guard by a backorder or a surge in usage.
- Compliance and Security: Healthcare organizations must maintain strict control over certain inventory, such as controlled substances, vaccines, or expensive medical devices. They face regulatory requirements for how such items are stored, logged, and secured. Lack of proper inventory management can result in non-compliance with laws (for example, missing records of a controlled drug) or even theft/diversion of high-value items if security measures are inadequate. Ensuring accountability and security for sensitive inventory is a constant challenge.
Recognizing these challenges is the first step toward improvement. The next step is implementing solutions and best practices to overcome them. Below are essential tips for managing clinic inventory effectively, addressing these common pain points and leveraging modern tools and strategies.
Essential Tips for Effective Clinic Inventory Management
1. Implement a Centralized Digital Inventory System
The foundation of efficient inventory management is a centralized system that tracks all stock in real time. Relying on scattered spreadsheets or separate logs in each department leads to incomplete and inconsistent information. Instead, clinics should adopt a dedicated inventory management system (software or application) where all inventory data is stored in one place and kept up to date. A centralized digital system provides a single source of truth – staff across procurement, pharmacy, nursing, and administration can all refer to the same current inventory levels. This visibility prevents situations where one department over-orders because they didn’t realize another department already had plenty in stock.
Modern inventory management software for healthcare allows tracking of every item’s quantity, location, and status from purchase to usage. By consolidating data, it becomes easier to analyze usage patterns and identify inefficiencies. For example, if a particular type of surgical supply is consistently underused in one clinic location, the central system might flag it so the staff avoids ordering more unnecessarily. A unified system also supports better supply chain resilience. When inventory information is connected across the clinic or multiple sites, managers can quickly reallocate stock between locations to prevent shortages in one area. In essence, a centralized inventory platform ensures that everyone “sees” the same inventory picture, enabling coordinated decision-making and reducing communication gaps.
Implementing such a system might involve using a cloud-based inventory application or integrating an inventory module into the clinic’s existing healthcare management software. Cloud-based solutions are especially useful for multi-site healthcare businesses, as they sync data instantly across all locations. Whichever solution is chosen, ease of use is crucial – staff should be able to log inventory transactions (like receiving items or using items) with minimal hassle. In summary, moving away from disjointed manual tracking to one comprehensive clinic inventory management system is the first and most important step to gain control over medical supplies.
2. Organize and Label All Stock Items
An often overlooked but vital inventory practice is maintaining physical organization and clear labeling of all items. Even with great software, the benefits are lost if supplies in storage are chaotic or mislabeled. Clinics should establish a tidy, logical arrangement for their stock rooms, pharmacy shelves, and equipment storage areas. This might mean grouping similar items together, designating specific shelves or bins for particular categories, and keeping a well-documented layout of storage locations. Good organization prevents items from “disappearing” on a back shelf and being reordered unnecessarily. It also helps staff find what they need quickly, which is crucial during busy clinic hours or emergencies.
Each inventory item should be clearly labeled with key information. For consumables and medications, use labels or barcode stickers that include the item name, stock-keeping unit (SKU) or code, and if applicable, an expiration date or lot number. For reusable medical equipment, tagging with barcodes or RFID tags is highly beneficial. Using barcode scanners or RFID readers in tandem with the inventory system lets staff check items in and out easily and update counts without manual data entry. Labeling and tagging not only improve accuracy but also deter loss or theft – it’s harder for equipment to go missing when everything is tagged and logged. As a best practice, assign someone to routinely audit the storage areas for orderliness and correct labeling, especially after hectic periods when things may be put back in the wrong place.
By organizing inventory physically and using a standardized labeling/tagging scheme, clinics avoid a major cause of redundancy. Misplacement of supplies is a common issue that leads to duplicate orders (because staff believe an item is out of stock when it is actually just stored incorrectly). Simple steps like alphabetized shelving for medications, color-coded bins for different categories, and barcode labels for each product can dramatically reduce such errors. In short, an orderly inventory is an efficient inventory – invest time in setting up a neat storage system and maintaining that order daily.
3. Track Inventory in Real Time with Technology
Leveraging technology for real-time inventory tracking can save a clinic from the pitfalls of delayed or inaccurate information. Instead of updating stock levels only at the end of the week or month (periodic manual counts), a real-time or perpetual tracking approach records every inventory transaction as it happens. This is made possible by inventory management software combined with tools like barcode scanners or RFID tags on products. For instance, when a nurse uses a vial of vaccine, scanning its barcode can instantly deduct it from the available inventory count. This immediacy ensures that the system’s data always reflects actual on-hand quantities.
Real-time tracking is crucial for avoiding surprises like sudden stockouts. It enables automated low-stock alerts: the system can be configured to send notifications (or even trigger automatic reorders) whenever an item’s quantity falls below a defined threshold. Relying on memory or infrequent manual checks is risky—staff might forget to reorder a rarely used item until it’s completely gone. Automated alerts act as a safety net, especially for high-turnover consumables such as gloves, test strips, or injection syringes. Many clinics start by setting up alerts for their most essential and fast-moving supplies, then gradually extend this to a wider range of items.
Using technologies like RFID and barcode scanning also significantly reduces human error. Each scan ensures accurate data capture (no typos or missed entries), and inventory records update instantly across the system. This level of accuracy is not just operationally beneficial; it also supports compliance by providing an audit trail for each item. For example, if a certain batch of medication is recalled by the manufacturer, a real-time system can quickly identify how many units of that batch are in stock and exactly where they are located. In short, real-time tracking gives clinics both the agility to respond quickly (preventing stock crises) and the accuracy needed for patient safety and regulatory compliance.
4. Use First-Expired, First-Out (FEFO) and Monitor Expiration Dates
Healthcare inventories include many time-sensitive items like medications, vaccines, reagents, and sterile supplies. To minimize waste and protect patients, clinics should rigorously follow FIFO (First-In, First-Out) and especially FEFO (First-Expired, First-Out) inventory methods. FIFO means that older stock (earliest received) is used before newer stock, which prevents items from sitting until they become obsolete. FEFO goes a step further by ensuring that the item with the nearest expiration date is used first, regardless of when it was purchased. This is particularly vital for pharmaceuticals and perishable medical supplies.
Implementing FEFO in practice requires two things: tracking expiration dates in the inventory system and organizing storage accordingly. Staff should record the expiration date of each batch or lot of products when logging them into inventory. The software can then flag items that are nearing expiration, or generate reports of items expiring in the next 30/60/90 days. In the physical storage, arranging products by expiry date (with soonest-to-expire items placed at the front of the shelf or bin) makes it intuitive for staff to pick the right item first. It’s also wise to perform regular inventory audits focused on expirations—perhaps a quick monthly sweep to pull any items due to expire in the next couple of months, so they can be used promptly or returned to the supplier if possible.
By using these methods, clinics can dramatically reduce the amount of expired stock that must be thrown away. This directly saves money and ensures that patients never receive outdated medicine or materials. It’s worth noting the scale of this issue: a significant percentage of medical inventory in the healthcare industry expires on shelves unused. In a small clinic, that might translate to a smaller absolute quantity but still represents avoidable cost and risk. Through diligent expiry tracking and a “first-expire, first-out” practice, healthcare facilities maintain a safer and more cost-effective inventory. Many modern inventory systems provide automatic alerts or dashboard indicators for items approaching expiration, which is very useful for busy clinics to stay on top of this task.
5. Set Par Levels and Reorder Points Based on Demand
Every clinic should determine par levels for critical supplies – essentially the minimum and optimum quantities to keep on hand for each item. Par levels should be set based on historical usage rates, supplier lead times, and a safety buffer for emergencies. For example, a clinic might decide it should always have at least 100 units of a certain disposable item in stock (the minimum), but not more than 300 units (to avoid excess). By defining these thresholds, the inventory management system can assist in maintaining optimal stock levels. When inventory falls below the minimum, it signals that it’s time to reorder; when it rises above the maximum, it indicates overstock that may need review (perhaps orders can be reduced for a while).
Optimizing reorder points is closely tied to this. Instead of ordering reactively when something runs out, proactive inventory management means ordering at the right time before an item is completely depleted. Using data from your system, you can configure reorder points that account for how quickly an item is used and how long it takes for new stock to arrive. For instance, if a particular reagent is used at a rate of 50 per week and the supplier’s delivery lead time is two weeks, a logical reorder point might be when the stock hits around 100 units (about two weeks’ supply remaining). This way, the new shipment arrives just as the clinic is running low, avoiding both last-minute shortages and excessive stockpiling.
Analyzing usage trends is important when setting these levels. Some items might have seasonal spikes (for example, flu vaccine demand increases in autumn), or occasional surges due to specific events (like a health camp or a local outbreak). Adjust par levels accordingly so that you’re prepared for predictable increases in demand. The goal is to avoid both stockouts and overstock through smart planning. Lean inventory principles, borrowed from supply chain management, can be applied here: keep inventory as low as possible without compromising availability. This practice leads to more efficient use of storage space and capital. In the long run, maintaining well-calibrated par levels and reorder points will simplify ordering routines and prevent the panic of emergency restocking.
6. Leverage Data Analytics for Forecasting and Optimization
In the age of data-driven decision making, even clinics can benefit from analytics to refine their inventory management. Modern inventory systems often include reporting and analytics tools that turn raw transaction data into useful insights. For example, dashboards can display usage trends for each category of item, highlight which supplies are used most (or least) frequently, and identify anomalies (like a sudden spike in usage of a particular item). By reviewing these patterns, clinic administrators can make informed decisions, such as adjusting order frequency or identifying opportunities to reduce waste.
Forecasting is one of the most valuable applications of analytics. Using historical data, a clinic can project future demand for supplies with greater accuracy. If you know that last year the clinic saw a 20% increase in patient volume during a certain month, or that a new specialized service will be offered soon, you can forecast an increased usage of related supplies and stock up accordingly. Predictive analytics, sometimes aided by artificial intelligence (AI) and machine learning, can factor in multiple variables (seasonality, growth trends, supplier reliability, etc.) to suggest optimal inventory levels and ordering schedules. Some advanced systems even predict the likelihood of shortages or delays for certain items and recommend preemptive actions before a problem occurs.
Data analytics also supports budgeting and cost optimization. With clear reports on inventory expenditures by department or by item, a healthcare business can pinpoint where money is going and identify cost-saving opportunities. For instance, analytics might reveal that one department consistently uses more of a particular supply per procedure than others, indicating a need to standardize protocols or provide training to reduce waste. Or it may show that a certain expensive medication often expires before use, prompting a change in ordering quantity or frequency.
Overall, harnessing inventory data turns management from a purely reactive task into a proactive strategy. Instead of relying on guesswork or memory, clinics use evidence to drive decisions. This not only ensures better availability of items but can significantly reduce costs associated with over-ordering or emergency procurement. In essence, treating inventory data as a strategic asset helps healthcare businesses continuously improve their operations and adapt to changes with confidence.
7. Assign Clear Responsibilities and Train Staff
An inventory management system is only as good as the people using and managing it. Clinics should clearly assign roles and responsibilities for inventory tasks. This means designating who will perform regular stock audits (cycle counts), who will place routine orders, who will receive deliveries and update the system, and who will investigate discrepancies. In a small practice, one person might wear multiple hats, but it’s still important to define these duties so nothing is overlooked. When everyone assumes “someone else” is keeping track of inventory, that’s when things fall through the cracks. By contrast, when specific team members know that inventory management is a defined part of their job, they are more likely to take ownership of it.
Training is equally crucial. All relevant staff should be trained on how to use the inventory management software and on the standard operating procedures for handling inventory. For example, train nurses and technicians to always record or scan items when they take supplies for use, or to log new deliveries into the system immediately upon receipt. Provide guidance on how to properly label new stock and where to store it according to the organizational scheme. If the clinic implements a new process like RFID tagging or a barcode system, take time to educate the team on why it’s important and how to use the new tools correctly. Periodic refresher training can help reinforce good practices, especially if there are updates to the system or if audits reveal consistent errors (such as items not being logged out properly).
Establishing a culture of accountability around inventory can also involve setting up checks and balances. For instance, one staff member could conduct a monthly spot-check of a few items (cycle counting) to verify that physical counts match the system, providing a second layer of oversight that can catch issues early. When discrepancies or issues are found, treat them not as individual blame but as a signal to improve the process or provide additional training. Keep in mind that efficient medical inventory management benefits everyone: it reduces the stress on staff who no longer have to scramble for missing items, helps clinicians trust that what they need will be available, and ultimately ensures patients receive timely care. By empowering and educating the team, a clinic ensures that its inventory system functions smoothly day-to-day, not just on paper.
8. Maintain Good Supplier Relationships and Backup Options
Suppliers are a key part of the inventory equation. A clinic could have an excellent internal system but still run into trouble if a supplier fails to deliver on time or sends subpar products. It’s wise for healthcare businesses to actively manage their vendor relationships and have contingency plans. Keep track of supplier performance in terms of delivery times, reliability, and quality of items delivered. For example, note if a distributor frequently ships late or only partially fulfills orders. Maintaining a simple vendor scorecard or log can highlight if one supplier’s service is slipping. With this information, a clinic can address issues with the vendor early (through communication or renegotiation) or decide to switch to a more dependable source if needed.
It’s also beneficial to diversify sources for critical supplies whenever possible. Relying on a single supplier for a vital item is risky—if that supplier has a stock shortage or logistic issue, your operations could be jeopardized. Where feasible, identify secondary suppliers (or maintain a small emergency reserve) for life-saving or high-turnover items. Recent global supply chain disruptions in healthcare have underscored the importance of having backup suppliers and a flexible procurement strategy. Some clinics form group purchasing arrangements or use local vendors as alternates when their primary suppliers face shortages, ensuring they have multiple avenues to obtain key supplies.
Another tip is to negotiate clearly with suppliers about inventory needs and even consider consignment stock arrangements. In a consignment inventory model, a supplier keeps a certain amount of stock on the clinic’s premises (or guarantees availability) but the clinic only pays for it when it’s used. This can act as a buffer for important items without tying up the clinic’s capital. Not all suppliers offer this, but it’s worth exploring for expensive implants or rarely used emergency drugs that you want on hand. Additionally, maintain open communication: inform your suppliers about your usage patterns and upcoming needs (e.g., if you expect an increase in patients or a new service launch that will require more supplies). In turn, ask them to alert you to any known supply issues or substitutions well in advance.
In summary, robust supplier management helps prevent inventory surprises from the supply side. It complements internal inventory control by ensuring that when a reorder is needed, the items will actually be available as expected. Building good relationships with vendors, understanding their limitations, and planning for the unexpected will make a clinic’s supply chain much more resilient against disruptions.
9. Ensure Security, Compliance, and Accountability
Healthcare inventories often include items that require special oversight and security. Controlled medications, for example, must be handled in accordance with strict regulations and documented meticulously to prevent misuse. Valuable medical devices or sensitive items (like needles or prescription pads) also need protection against theft or loss. A good clinic inventory management system will incorporate features like role-based access control and audit logs to enhance security and accountability. This means not every employee can access or modify all inventory records – permissions are set so that individuals only handle the parts relevant to their role. For instance, a nurse might be allowed to log the usage of supplies in the system, but only a pharmacist or manager can approve new orders or adjust inventory counts for medications. Such controls reduce the risk of internal pilferage or accidental misrecording, and also protect confidential data.
Auditability is another important aspect. The system should automatically log who performed each inventory transaction and when (for example, recording that User X removed 5 units of medication Y on a certain date/time). These logs create a traceable audit trail and can be critical if an investigation is needed – if a controlled drug count doesn’t add up, the system’s log shows who last accessed it and subsequent steps can be taken to resolve the discrepancy. Many clinics also conduct routine audits of high-risk inventory (such as weekly counts of opioids or monthly checks of expensive equipment) as an extra precaution. Ensuring that processes and software support these audits and record-keeping will help the clinic stay compliant with regulations and accreditation standards that require strict inventory control.
Compliance extends to digital security and privacy as well. While an inventory system primarily tracks supplies, if it integrates with patient billing or electronic health records it may handle sensitive patient information. In such cases, the system must be compliant with healthcare data privacy laws (like HIPAA in the U.S. or GDPR in Europe) and employ strong cybersecurity measures (encryption, secure login, regular backups) to protect against data breaches. Even without patient data, protecting the integrity of inventory data is important – a ransomware attack or major data loss could cripple the clinic’s operations by leaving it uncertain about its supply counts.
In essence, this tip is about embedding strong governance into inventory management. By using system features and workplace policies that enforce security, compliance, and accountability, a healthcare business builds trust with regulators and patients. It demonstrates that the clinic knows exactly where its critical supplies are, that only authorized personnel can handle certain high-stakes items, and that there is transparency in inventory operations. All of these factors contribute to safer healthcare delivery and a more trustworthy organization.
10. Integrate Inventory Management with Other Systems
To fully unlock efficiency, inventory management should not exist in isolation. Integrating the inventory system with other key systems in the clinic can streamline workflows and reduce duplicate work. For instance, linking your inventory software with the electronic health record (EHR) or practice management system can automatically tie inventory usage to patient care events. When a medication or a medical supply is used for a patient (during a procedure or consultation), the system can deduct it from inventory and simultaneously record the usage in the patient’s record or the billing system. This not only saves staff from having to enter the same information in multiple places, but it also improves billing accuracy – every item used in patient care is accounted for and charged appropriately, and patient bills reflect the actual supplies consumed.
Integration with accounting and purchasing systems is also highly beneficial. If the inventory management system connects with the clinic’s procurement or ordering system, it can automatically generate purchase orders when stock is low, which then can be reviewed and sent to suppliers with minimal manual effort. Similarly, when ordered goods are received, the inventory system can update stock levels and inform the accounts payable that an invoice can be expected, creating a smooth procure-to-pay workflow. Many clinics find value in integrating inventory data with their financial systems to track supply expenses in real time and to calculate more accurate costs for services (for example, knowing exactly how much each type of procedure costs in supplies).
Another important integration point is with maintenance or asset management systems. For clinics that utilize a lot of biomedical equipment or run in-house laboratories, linking the inventory of consumables (like test cartridges, reagents, spare parts) with equipment maintenance schedules can be very useful. The inventory system can trigger reorders for lab reagents when it sees that upcoming scheduled tests will consume the remaining stock, or alert technicians to restock an MRI machine’s supplies before a busy week of appointments. Integration ensures that each part of the operation that uses supplies is communicating with the inventory control in real time.
In summary, breaking down silos between the inventory management system and other software results in an interconnected healthcare IT ecosystem. The payoff is increased efficiency, fewer administrative errors, and richer data for decision-making. When evaluating inventory management solutions, healthcare businesses should look for platforms that offer integration capabilities (APIs or built-in connectors) to the systems they already use (such as EHR, pharmacy management, billing, or procurement platforms). This will make the inventory system a seamless part of the clinic’s workflows and amplify the benefits of having a dedicated system, since information flows easily from one part of the operation to another.
Conclusion
Efficient inventory management is a linchpin of success for healthcare businesses. By implementing the essential tips outlined above – from centralizing and digitizing your inventory data to training staff and using analytics – clinics can greatly enhance their operational efficiency and ensure that patient care is never disrupted by supply issues. A well-managed inventory means clinicians have what they need when they need it, budgets are protected through waste reduction, and the organization can smoothly adapt to changes or even emergencies. In a competitive healthcare landscape, having superior control over resources also becomes a strategic advantage. It enables facilities to provide reliable care (leading to a better reputation and patient trust) and to run leaner, more cost-effective operations.
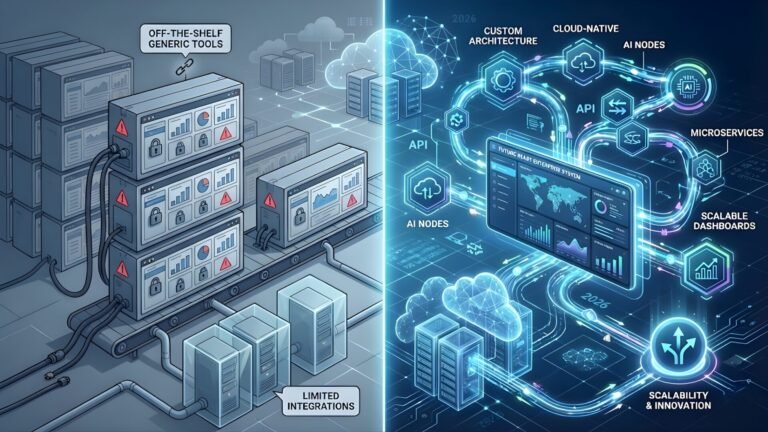
One powerful way to achieve these benefits is by leveraging a custom inventory management app tailored to the clinic’s specific workflows. While off-the-shelf software can work, a custom solution can be designed to integrate seamlessly with existing processes – whether it’s syncing with appointment scheduling and billing systems, accommodating unique inventory items, or generating specialized reports that management needs. Building a custom clinic inventory management system can significantly improve operational efficiency, giving the business a competitive edge through technology. It ensures the clinic is not forced to adapt its processes to a generic tool; instead, the tool is built to fit the clinic’s processes.
Flutebyte Technologies offers a broad range of IT services, including professional web development, custom software solutions, Shopify development, SaaS platform development, and more – all delivered at minimal cost with expert support. Healthcare organizations can contact Flutebyte Technologies to discuss the development of a bespoke inventory management application tailored to their needs. With the right technological partner, even a small clinic can deploy a powerful system that improves efficiency and provides a competitive advantage. Flutebyte’s team stands ready to assist in building such solutions, allowing healthcare providers to boost operational performance and focus on delivering excellent patient care.
FAQs
Q1: What is a clinic inventory management system?
A: It is a software tool or platform designed to help healthcare facilities track and control their medical supplies, medications, and equipment. A clinic inventory management system provides a centralized database of all stock items along with details like quantities on hand, storage locations, and expiration dates. It often includes features such as barcode/RFID scanning for easy logging, automated alerts for low stock or expiring items, and reporting dashboards. By using such a system, clinics can ensure they have the necessary supplies available, prevent shortages or overstock situations, and maintain accurate records of inventory transactions in real time.
Q2: Why is inventory management important for healthcare businesses?
A: Effective inventory management is crucial in healthcare because it directly affects patient care and operational costs. Proper management ensures that essential medical items (like drugs, IV fluids, gloves, or diagnostic kits) are always available when needed, thereby avoiding treatment delays or cancellations due to missing supplies. It also helps maintain patient safety by making sure expired or recalled products are promptly removed and never used in care. From a business perspective, good inventory control prevents wasteful spending on excess supplies that might expire unused and reduces last-minute emergency purchases, thereby improving the facility’s financial efficiency. In short, well-managed inventory supports uninterrupted clinical operations, compliance with health regulations, and better overall quality of service.
Q3: How can clinics improve their medical inventory management?
A: Clinics can take several practical steps to enhance their medical inventory management. First, adopting a digital inventory management system in place of paper logs or spreadsheets will provide better real-time tracking and accuracy. Second, implementing organization and labeling best practices – for example, keeping stockrooms orderly, labeling every item or box with clear names and dates, and segregating products by category – makes it easier for staff to find and monitor supplies. Clinics should also use methods like First-Expired, First-Out (FEFO) to ensure older supplies or those nearing expiration are used before newer ones, reducing waste. Setting minimum (par) stock levels and utilizing automated reordering alerts can ensure timely replenishment of critical items. Regular training for staff on inventory procedures and periodic audits (stock counts) will help catch errors or discrepancies early. By combining these approaches, clinics can greatly improve the visibility, efficiency, and reliability of their inventory management.
Q4: What features should an inventory management system have for clinics?
A: An ideal inventory management system for a clinic should have features tailored to healthcare needs. Key features include real-time tracking of stock levels, so that any changes (like usage or new deliveries) are instantly reflected. Integration of barcode or RFID technology is important for quick and accurate logging of items moving in or out. The system should provide alert functions for low stock thresholds and upcoming expiration dates to prompt timely action. It’s also valuable for the software to support integration with other systems – for example, linking with electronic health records, billing, or procurement systems – to streamline workflows (like automatic deduction of supplies when used for a patient, or generating purchase orders when stock is low). Role-based user access control is another crucial feature, which ensures that only authorized staff can perform sensitive actions (such as adjusting controlled drug inventory or approving orders), thereby maintaining security and compliance. Lastly, robust reporting and analytics capabilities help in reviewing usage patterns, forecasting demand, and making data-driven decisions to continuously optimize the inventory.
Q5: How can a custom inventory management app benefit a healthcare clinic?
A: A custom-built inventory management application can offer numerous benefits to a healthcare clinic by addressing its specific challenges and workflows. Because the app is tailored to the clinic’s processes, it can integrate seamlessly with existing systems (like the clinic’s patient management or billing software) and be designed to track the exact categories of inventory the clinic uses. This means the clinic doesn’t have to adapt to a one-size-fits-all solution – the software fits them. A custom app can include specialized features that off-the-shelf products might not provide, such as custom reports relevant to the clinic’s KPIs, modules for particular departments (pharmacy, lab, etc.), or compliance checks specific to local regulations. It can also be scaled according to the clinic’s size and growth, ensuring that as the business expands or changes, the app can be updated to meet new requirements. In terms of competitive advantage, having a well-tuned inventory system helps a clinic reduce waste and costs, avoid supply shortages (which improves reliability and patient trust), and save staff time through automation. While developing a custom app requires an upfront investment, the long-term gains in efficiency, accuracy, and adaptability can be significant – often resulting in cost savings and better service quality that outweigh the development cost.
Sources
- MedCity News – “Protect Shrinking Margins With Supply Chain Data.” (Feb 2023). MedCityNews.com
- NetSuite Blog – “8 Best Practices for Hospital Inventory Management.” (Feb 2025). NetSuite.com
- MedPak (MPI) – “Hospital Inventory Management Best Practices.” (2024). MedPak.com
- Blaze.tech Blog – “Healthcare Inventory Management Guide: +6 Best Practices.” (Jun 2025). Blaze.tech
- Enerpize – “Benefits of Using Inventory Management Software for Medical Clinics.” (Jul 2024). Enerpize.com